Blaivas (Am J Emerg Med 2006;24:293) 30 cc of 1% lidocaine or 0.25% bupivicaine 20 G spinal needle (non-cutting is safer around nerves) 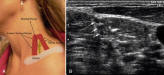
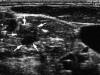


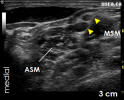

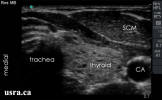

 If the angle is steep (>45), it will not show up well in long access. Either lower the angle or use a bigger needle (17G). Use short bevel to lower trauma Have head turned 45 degrees away from you 2-3 cm down Carotid to IJ to ASM to nerve roots Just deep to
If the angle is steep (>45), it will not show up well in long access. Either lower the angle or use a bigger needle (17G). Use short bevel to lower trauma Have head turned 45 degrees away from you 2-3 cm down Carotid to IJ to ASM to nerve roots Just deep to
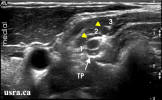
the tip of the SCM, but if head is not turned adequately, the SCM will overlay the groove 5 cm 22 g needle Inject between the top and middle root Scan down into the supraclav region and trace the nerves up if having trouble identifying them Nerves run c5-c7 shallow to deep Uts guided 5cc as effective as 20 cc c less side effects (Br J Anaesth 2008; 101: 54956) my take is to use 10 cc 2% lido with 1 cc of bicarb added inject it between c5 and c6 nerve
Interscalene Block
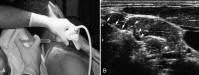
Clinical Applications The principal indication for interscalene block is surgery on the shoulder. Blockade occurs at the level of the upper and middle trunks. Although this approach can be used for forearm and hand surgery, blockade of the inferior trunk (C8 through T1) is often incomplete and requires supplementation at the ulnar nerve for adequate surgical anesthesia in that distribution. [8] Technique The brachial plexus shares a close physical relationship with several structures that serve as important landmarks for the performance of interscalene block. In its course between the anterior and middle scalene muscles, the plexus is superior and posterior to the second and third parts of the subclavian artery. The dome of the pleura lies anteromedial to the inferior trunk. This technique can be performed with the patient’s arm in any position and is technically simple because of easy identification of necessary landmarks. [ 9] The patient should be in the supine position, with the head turned away from the side to be blocked. The posterior border of the sternocleidomastoid muscle is readily palpated by having the patient briefly lift the head. The interscalene groove may be palpated by rolling the fingers posterolaterally from this border over the belly of the anterior scalene muscle into the groove. A line is extended laterally from the cricoid cartilage to intersect the interscalene groove, indicating the level of the transverse process of C6. Although the external jugular vein often overlies this point of intersection, it is not a constant or reliable landmark. The use of a nerve stimulator or elicitation of paresthesias is recommended with this technique to place the local anesthetic solution accurately. After ordinary sterile precautions and injection of a skin wheal, a 22- to 25-gauge, 4-cm needle is inserted perpendicular to the skin with a 45-degree caudad and slightly posterior angle ( Fig. 44-3 ). The needle is then advanced until a paresthesia (usually C5 and C6 dermatomes) or nerve stimulator response is elicited. This usually occurs at a very superficial level. Paresthesia or motor response of the arm or shoulder is equally efficacious. [10] If a blunt needle bevel is used, a “click” may be detected as the needle passes through the prevertebral fascia. If bone is encountered within 2 cm of the skin, it is likely to be a transverse process, and the needle may be “walked” across this structure to locate the nerve. Likewise, contraction of the diaphragm indicates phrenic nerve stimulation and anterior needle placement; the needle should be redirected posteriorly to locate the brachial plexus. After the appropriate paresthesia or motor response is obtained, the needle is stabilized. The use of flexible extension tubing facilitates the maintenance of the needle position while aspiration and injection occur. After negative aspiration, 10 to 40 mL of solution is injected incrementally, depending on the desired extent of blockade. Radiographic studies suggest a volume-to-anesthesia relationship, with 40 mL of solution associated with complete cervical and brachial plexus block. [9] Clinical studies, however, indicate variable blockade of the lower trunk (i.e., ulnar nerve) even with large volumes of solution. [8] Digital pressure above the injection site and downward massage along with a 45-degree head-up position may facilitate caudad spread and blockade of the lower trunk. Side Effects and Complications Ipsilateral phrenic nerve block resulting in diaphragmatic paresis occurs in 100% of patients undergoing interscalene blockade,[ 11] even with dilute solutions of local anesthetics, and is associated with a 25% reduction in pulmonary function.[ 12] [13] This effect probably results from anterior spread of the solution over the anterior scalene muscle and may cause subjective symptoms of dyspnea. Although rare, respiratory compromise can occur in patients with severe respiratory disease. Involvement of the vagus, recurrent laryngeal, and cervical sympathetic nerves is rarely significant, but the patient experiencing symptoms related to these side effects may require reassurance. The risk of pneumothorax is low when the needle is correctly placed at the C5 or C6 level because of the distance from the dome of the pleura. Severe hypotension and bradycardia (i.e., Bezold-Jarisch reflex) have been reported in awake, sitting patients undergoing shoulder surgery under an interscalene block. The cause is presumed to be stimulation of intracardiac mechanoreceptors by decreased venous return, producing an abrupt withdrawal of sympathetic tone and enhanced parasympathetic output. This effect results in bradycardia, hypotension, and syncope. The frequency is decreased when prophylactic â-blockers are administered. [14] Nerve damage or neuritis can occur in any peripheral nerve block, but it is uncommon and usually is self-limited. Some surgical approaches to the shoulder, such as total shoulder arthroplasty, are associated with neurologic risk to the brachial plexus. [15] In such cases, an interscalene block should be placed postoperatively for pain relief after the surgical service has ascertained and documented that no neurologic damage has occurred. Epidural and intrathecal injections have been reported with this block, a finding emphasizing the importance of inserting the needle in a caudad direction. The proximity of significant neurovascular structures may increase the risk of serious neurologic complications when interscalene block is performed in heavily sedated or anesthetized patients. [16] Several vascular structures are in proximity to a correctly placed needle. Local anesthetic toxicity as a result of intravascular injection should be guarded against by careful aspiration and incremental injection. Seizure activity from this complication is particularly undesirable after rotator cuff surgery, because the repair can be compromised by the associated muscular activity. Anesthes July 2006 In theory, for a needle to gain access through the intervertebral foramen into the neuraxis during an ISBPB, it must be sufficiently long, it must be directed toward the foramen, and its approach angle should approximate to the exit angle of the foramen. The question posed by this study is as follows: Does the classic interscalene block technique for ISBPB pose the greatest risk of needle passage into the neuraxis in terms of all the three above requirements? The first consideration is needle length and the depth from the skin of the intervertebral foramen. Given that the C6 root is the accepted target of an ISBPB, the important data in this respect are the distances between the three markers and the C6 intervertebral foramen. The classic interscalene approach marker (marker 3) left the skin at a median (range) distance from the intervertebral foramen of 3.7 (2.55.9) cm. This implies that if a 5-cm needle is used, the intervertebral foramina of the majority of patients could be reached using the classic interscalene approach. A 2.5-cm needle has been recommended in the literature.16 If a 2.5-cm needle were used, it would still be possible in some patients to insert the needle into the intervertebral foramen, especially if the skin were indented by the anesthesiologists finger resting, for example, on the interscalene groove. The distance data for marker 1 and marker 2 are 4.3 (3.45.6) and 3.9 (3.35.3) cm, respectively. These data suggest, but do not conclusively prove, that it would be difficult to gain access to the intervertebral foramen with a 2.5-cm using these approaches in some patients, although a 5-cm needle would be able to reach the foramen in the majority of patients. However, when using higher approaches, it is possible that the distance between the skin and the upper root of the brachial plexus may be more than 2.5 cm, thereby mandating the use of a 5-cm needle. The second consideration is whether the needle is directed toward the intervertebral foramina in traditional ISBPB approaches. Winnies original description of the needle angle was vague: mostly medial but slightly posterior and slightly caudad.2 Our data suggest that the median (range) caudal angle that would allow needle access to the intervertebral foramen of the C6 vertebra is 6.8° (-9.9° to 26.8°), i.e., slightly caudad for the majority of patients. However, a needle angulation of greater than 30° would seem to ensure that the needle will pass below the C6 foramen. However, the cricoid landmark is not a reliable guide to vertebral level and may lie anywhere between the C5 and C7 levels.17 The caudal angle necessary to gain access to the C7 intervertebral foramen from the classic interscalene entry point (marker 3) was 28.8° (15.9°46.9°), which suggests that a caudal angle greater than 50° would ensure that the needle passes below the C7 foramen. The third consideration is whether the needle approach angle, i.e., the vector of the needle during its insertion, is in alignment with the exit angle, i.e., the vector at which the nerves are exiting from the intervertebral foramen. It is likely that the smaller this angle is, and therefore the greater the degree of alignment is, the greater the chance is that the needle can pass into the foramen. Again, taking the C6 vertebra and the three approaches determined by the three markers, the greatest degree of alignment, i.e., the smallest discrepancy angle, is seen with the classic interscalene approach (marker 3). The median (range) discrepancy angle for the classic interscalene approach to the C6 vertebra is 29.6° (18.6°66.0°), the smallest discrepancy angle for the three approaches to any of the five cervical vertebrae studied. There is a question of whether the extent to which the neck is turned before insertion of the needle affects the needle entry angles relative to the spine. Our data suggest that when a healthy patients neck is turned in preparation for an ISBPB, there is little rotation (turn angle) at the vertebrae in the target area for the block, and hence this factor is unlikely to affect the needle angles. Our results seem to be supported by a study performed by Wong et al.,15 who calculated the ideal needle angle to access the upper roots of the brachial plexus with a traditional ISBPB entry point at the C6 vertebral level. Using magnetic resonance images, they calculated that the median (range) ideal angle relative to the sagittal plane was 61.1° (50°78°). Two points arise from the article of Wong et al.. First, this angle is similar to the C6 intervertebral foramen angle that we measured (50.4° [40.0°65.4°]). Second, the illustration in the article of Wong et al. of the ideal angle shows the needle path passing through the spinal cord. The introduction to this article posed the question of whether the traditional classic interscalene approach for ISBPB aligned the needle path necessary to reach the upper roots of the brachial plexus with the path that would allow passage of the needle through the intervertebral foramen and into the spinal canal. The answer to this question that emerges from our data, albeit from a small study, is that the alignment is not perfect and that a competently performed classic interscalene ISBPB with a short (2.5 cm) needle should not pose a threat to a patients neuraxis. However, of the three needle approaches studied, represented by the three markers, the classic interscalene approach (marker 3) creates the greatest degree of alignment. Does this conclusion mean that the classic interscalene approach is unsafe and should be abandoned in favor of more proximal entry points? The answer is not simple. The classic interscalene approach has been used for many years and seems to be safe in the hands of an experienced, competent practitioner. Currently, there are no clinical data to suggest that it is more unsafe than the proximal approaches. However, not all practitioners are experienced and competent, and we think that our data adds support to the view that a more proximal ISBPB approach with a markedly caudad needle angle offers the patient a greater degree of protection against entry into the spinal cord from regional anesthetic practice that falls short of ideal. Whether a higher approach needing a direction of needle more parallel to the cervical spine can increase the risk of other complications such as pneumothorax remains unanswered with this study. 


 deltoid twitches or twitches below the shoulder are good hiccups or trapezius twitches are not no paresthesia=no anesthesia 100% ipsilateral phrenic block, pts must be able to tolerate 25% reduction in pulmonary function possible recurrent laryngeal nerve block, giving hoarseness. Do not use if pt already has one vocal cord paralyzed only 6 cases in the world literature of permanent brachial plexus injury from scalene block, one case had severe paresthesia on needle placement, but injection was still continued. Other five cases had block placed under general anesthesia Infraclav Simon Lévesque, MD, Nicolas Dion, MD and Marie-Christine Desgagné, MD CHA Hôpital Enfant-Jésus, Québec City, Canada, E-mail: simlevesque@hotmail.com To the Editor: We congratulate Dr. Morimoto et al.1 for their excellent work demonstrating the existence of a septum that restricts the diffusion of local anesthetic (LA) during ultrasound-guided infraclavicular block. This study confirms our clinical impression that a septum, or a fascia, must be pierced on the posterolateral aspect of the subclavian artery (SA) to ensure a reliable block of the brachial plexus. At our institution, we perform ultrasound-guided infraclavicular block in a manner very similar to that described by Dr. Morimoto; however, we use a 20G Tuohy needle (BBraun, Bethlehem, PA, USA) and we aim to position the tip of the needle at the very posterior aspect of the SA before the injection. Using such a non-cutting needle allows us to consistently feel the passage of the posterolateral septum. In fact, this fascial click has become our primary endpoint to confirm a good needle position. We have observed that this technique strongly predicts a U-shaped distribution of the LA and an anterior displacement of the SA. In our practice, the combination of these three factors; fascial click, U-shaped distribution of LA, and anterior displacement of the SA, is highly predictive of a rapid and complete block of the entire arm. In contrast, if the fascial click is not perceived before the injection, even if the needle tip is posterior to the artery, a lateral distribution of the LA and a caudad or posterior displacement of the SA is often observed. This scenario often leads to an incomplete block, or to a delayed onset, before adequate anesthesia is achieved. The existence of this septum can explain why studies of neurostimulation-guided, infraclavicular block show better success rates, when administering injections on a posterior cord motor response, rather than on a medial or lateral cord motor response.2,3 It may also explain the findings of Dingemans et al.4 who demonstrated an excellent success rate when obtaining a U-shaped distribution of the LA. Sauter et al.5 recently reported an MRI study which delineates the position of the three cords in relation with the SA. Based on their observations, it is suggested that an optimal target point exists closest to all three cords on the posterolateral aspect of the SA.5 In our experience, using this injection point seldom pierces the septa and often leads to incomplete block. As anesthesiologists gain more knowledge regarding the anatomical relations of the brachial plexus with the use of ultrasound, it becomes clear that for regional anesthesia of the upper limb, we need to think in terms of the diffusion compartment, instead of focusing on pure needle-to-nerve distance. Maki Morimoto, MD, Jovan Popovic, MD, Jung T. Kim, MD, Harald Kiamzon, MD and Andrew D. Rosenberg, MD NYU Medical Center, New York, USA, E-mail: maki.morimoto@med.nyu.edu We sincerely thank Dr. Lévesque and his colleagues for their excellent comments. In particular, we were quite intrigued to learn about the “three factors” to predict the outcome of the infraclavicular brachial plexus blocks. At our institution, instead of making use of “three factors,” we utilize one common endpoint to ensure the success of the blocks. It is the deposition of the local anesthetic (LA) around the brachial plexus cords. We believe that having the LA “bathe” the nerves is important in predicting the success of the blocks. The U-shaped distribution of LA and the anterior displacement of the artery are often seen as a result of the correct deposition of the LA. Fascial click, however, is sometimes felt twice during the blocks. One click is always felt as the needle pierces the neurovascular sheath, and the second click is sometimes felt as it passes through the septum. Dr. Lévesque writes, “… we need to think in terms of the diffusion compartment, instead of focusing on pure needle-to-nerve distance”. We, too, feel that observing the appropriate LA spread is far more important than having the block needle near the nerve at the beginning of the block. Sinha et al.1 have previously reported that the presence of nerve stimulation had no impact on the success of the resulting blocks. Not only does the ultrasound technology allow us to locate the target structures, it also allows us to direct the needle and to observe the real-time LA spread. Ultimately, this know-how should lead to safer and more effective blocks. [6] D. Norris, A. Klahsen and B. Milne, Delayed bilateral spinal anaesthesia following interscalene brachial plexus block, Can J Anaesth 43 (3) (1996), pp. 303305. View Record in Scopus | Cited By in Scopus (16) [7] B.D. Sites, B.C. Spence and J.D. Gallagher et al., Characterizing novice behavior associated with learning ultrasound-guided peripheral regional anesthesia, Reg Anesth Pain Med 32 (2) (2007), pp. 107115. Article | PDF (321 K) | View Record in Scopus | Cited By in Scopus (8) [8] W.F. Urmey, K.H. Talts and N.E. Sharrock, One hundred percent incidence of hemidiaphragmatic paresis associated with interscalene brachial plexus anesthesia as diagnosed by ultrasonography, Anesth Analg 72 (4) (1991), pp. 498503. View Record in Scopus | Cited By in Scopus (133) If you use ultrasound, can you use less anesthetic (Br J Anaes 2008;101(4):549) they used 5% ropivacaine 0.5%
deltoid twitches or twitches below the shoulder are good hiccups or trapezius twitches are not no paresthesia=no anesthesia 100% ipsilateral phrenic block, pts must be able to tolerate 25% reduction in pulmonary function possible recurrent laryngeal nerve block, giving hoarseness. Do not use if pt already has one vocal cord paralyzed only 6 cases in the world literature of permanent brachial plexus injury from scalene block, one case had severe paresthesia on needle placement, but injection was still continued. Other five cases had block placed under general anesthesia Infraclav Simon Lévesque, MD, Nicolas Dion, MD and Marie-Christine Desgagné, MD CHA Hôpital Enfant-Jésus, Québec City, Canada, E-mail: simlevesque@hotmail.com To the Editor: We congratulate Dr. Morimoto et al.1 for their excellent work demonstrating the existence of a septum that restricts the diffusion of local anesthetic (LA) during ultrasound-guided infraclavicular block. This study confirms our clinical impression that a septum, or a fascia, must be pierced on the posterolateral aspect of the subclavian artery (SA) to ensure a reliable block of the brachial plexus. At our institution, we perform ultrasound-guided infraclavicular block in a manner very similar to that described by Dr. Morimoto; however, we use a 20G Tuohy needle (BBraun, Bethlehem, PA, USA) and we aim to position the tip of the needle at the very posterior aspect of the SA before the injection. Using such a non-cutting needle allows us to consistently feel the passage of the posterolateral septum. In fact, this fascial click has become our primary endpoint to confirm a good needle position. We have observed that this technique strongly predicts a U-shaped distribution of the LA and an anterior displacement of the SA. In our practice, the combination of these three factors; fascial click, U-shaped distribution of LA, and anterior displacement of the SA, is highly predictive of a rapid and complete block of the entire arm. In contrast, if the fascial click is not perceived before the injection, even if the needle tip is posterior to the artery, a lateral distribution of the LA and a caudad or posterior displacement of the SA is often observed. This scenario often leads to an incomplete block, or to a delayed onset, before adequate anesthesia is achieved. The existence of this septum can explain why studies of neurostimulation-guided, infraclavicular block show better success rates, when administering injections on a posterior cord motor response, rather than on a medial or lateral cord motor response.2,3 It may also explain the findings of Dingemans et al.4 who demonstrated an excellent success rate when obtaining a U-shaped distribution of the LA. Sauter et al.5 recently reported an MRI study which delineates the position of the three cords in relation with the SA. Based on their observations, it is suggested that an optimal target point exists closest to all three cords on the posterolateral aspect of the SA.5 In our experience, using this injection point seldom pierces the septa and often leads to incomplete block. As anesthesiologists gain more knowledge regarding the anatomical relations of the brachial plexus with the use of ultrasound, it becomes clear that for regional anesthesia of the upper limb, we need to think in terms of the diffusion compartment, instead of focusing on pure needle-to-nerve distance. Maki Morimoto, MD, Jovan Popovic, MD, Jung T. Kim, MD, Harald Kiamzon, MD and Andrew D. Rosenberg, MD NYU Medical Center, New York, USA, E-mail: maki.morimoto@med.nyu.edu We sincerely thank Dr. Lévesque and his colleagues for their excellent comments. In particular, we were quite intrigued to learn about the “three factors” to predict the outcome of the infraclavicular brachial plexus blocks. At our institution, instead of making use of “three factors,” we utilize one common endpoint to ensure the success of the blocks. It is the deposition of the local anesthetic (LA) around the brachial plexus cords. We believe that having the LA “bathe” the nerves is important in predicting the success of the blocks. The U-shaped distribution of LA and the anterior displacement of the artery are often seen as a result of the correct deposition of the LA. Fascial click, however, is sometimes felt twice during the blocks. One click is always felt as the needle pierces the neurovascular sheath, and the second click is sometimes felt as it passes through the septum. Dr. Lévesque writes, “… we need to think in terms of the diffusion compartment, instead of focusing on pure needle-to-nerve distance”. We, too, feel that observing the appropriate LA spread is far more important than having the block needle near the nerve at the beginning of the block. Sinha et al.1 have previously reported that the presence of nerve stimulation had no impact on the success of the resulting blocks. Not only does the ultrasound technology allow us to locate the target structures, it also allows us to direct the needle and to observe the real-time LA spread. Ultimately, this know-how should lead to safer and more effective blocks. [6] D. Norris, A. Klahsen and B. Milne, Delayed bilateral spinal anaesthesia following interscalene brachial plexus block, Can J Anaesth 43 (3) (1996), pp. 303305. View Record in Scopus | Cited By in Scopus (16) [7] B.D. Sites, B.C. Spence and J.D. Gallagher et al., Characterizing novice behavior associated with learning ultrasound-guided peripheral regional anesthesia, Reg Anesth Pain Med 32 (2) (2007), pp. 107115. Article | PDF (321 K) | View Record in Scopus | Cited By in Scopus (8) [8] W.F. Urmey, K.H. Talts and N.E. Sharrock, One hundred percent incidence of hemidiaphragmatic paresis associated with interscalene brachial plexus anesthesia as diagnosed by ultrasonography, Anesth Analg 72 (4) (1991), pp. 498503. View Record in Scopus | Cited By in Scopus (133) If you use ultrasound, can you use less anesthetic (Br J Anaes 2008;101(4):549) they used 5% ropivacaine 0.5%  they rec. blocking only the C5 and C6 roots to avoid phrenic involvement From Neuroaxiom.com
they rec. blocking only the C5 and C6 roots to avoid phrenic involvement From Neuroaxiom.com  conventional
conventional  Interscalene Block using Ultra-Low Local Volume Click on the picture to the right to see an animation Ultra-Low Volume Interscalene Block using 5-7 ml Directly into Brachial Plexus Sheath Fast Onset, Duration 8-12 hours with Long-acting anesthetic + epinephrine or clonidine Incidence of Paralyzed Hemidiaphragm ~22%
Interscalene Block using Ultra-Low Local Volume Click on the picture to the right to see an animation Ultra-Low Volume Interscalene Block using 5-7 ml Directly into Brachial Plexus Sheath Fast Onset, Duration 8-12 hours with Long-acting anesthetic + epinephrine or clonidine Incidence of Paralyzed Hemidiaphragm ~22%